This article talks about your friend Molly. It says that because of Fanconi anemia she would not live to see her 8th birthday. They used to tell us the same thing. Thankfully, Molly is alive and okay.
Today would have been your 9th birthday. I think they should have said because of Fanconi anemia you would not live to see your 8th birthday, and 9th and 10th and 11th and 12th and 13th. Just saying one of them doesn't really bring home the reality of it all.

Procedure opens window of hope
By JENNI LAIDMAN
Blade Science Writer
October 25, 2004
The box felt empty.
Still, its presence on the floor of the backseat weighed on Jennifer and Joe Makhlouf with the heft of a planet.
The Lambertville couple drove to Chicago with this strange little container in their care. They could hardly bear to touch it.
Inside the lunchbox-sized incubator were two tiny embryos.
Since the 1980s, researchers have sought a way to predict the genetic health of embryos before they're put in a woman's womb.
The Makhloufs are among hundreds of couples taking advantage of testing that they hoped would save them the grief of another miscarriage.
But the technique, called preimplantation genetic diagnosis, or PGD, is fraught with controversy. Some criticize its accuracy. Some worry about what happens when one or two cells of an eight-cell embryo are removed for analysis. And others worry about the morality of choosing a child based on the genes he possesses.
For the Makhloufs, the question was simple: were these embryos even sound enough to survive? But the technique has far more ethically complicated applications. Parents can select an infant's sex. They can screen out embryos with genetic childhood disease. They can select babies who won't develop ailments that occur far into adulthood, such as Huntington's disease or some forms of Alzheimer's. They can even use it to select an infant to save the life of another child.
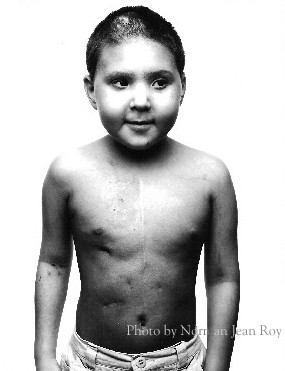
That's what Lisa and Jack Nash did. In 1999, the Denver couple's little girl Molly was dying of a rare genetic disease called Fanconi anemia. Without a stem-cell transplant from a matching donor, Molly's chances were slim.
"There was this gorgeous little baby, and they were telling us" she had the worst type of Fanconi, Lisa Nash said. Her bone marrow, with all its blood-making capabilities, would fail. Doctors said Molly wouldn't live to see her 8th birthday.
"In the back of my mind I'm thinking, yeah. Right. I don't care what I have to do, or where I have to go, she's going to make it. She's going to be OK," Lisa said.
Molly was born without hip sockets. She had no thumbs. She had holes in her heart and was deaf in her left ear. Eating was difficult. She had to be tube fed. Surgeries corrected her hands. She had multiple stomach operations. But by age 3, her bone marrow was failing.
When the Nashes heard about preimplantation diagnosis, it was with a bright stab of hope. Here was the chance to pick an embryo without Fanconi - there was a 1 in 4 chance any child of theirs would be born with the disease - that would be a genetic match for their little girl.
A child who was an immune-match would be a baby saver. After its birth, its umbilical cord blood would be collected, and the stem cells within would be grown to create new bone marrow for Molly. But four IVF attempts in 12 months failed. Lisa Nash had two miscarriages. Other embryos carried Fanconi, or lacked the right genetic signature.
It seemed hopeless. Even their doctor counseled against a fifth attempt. But Lisa insisted. This time, Lisa's eggs made only three embryos. Two were bone marrow matches. One of those matches had Fanconi.
"So we have one. This is our last shot," she said.
She had the embryo put into her womb, and continued to watch Molly fail day by day. It didn't look good.
On Christmas Eve, 1999, the doctor's office called and told her she was pregnant. Lisa didn't believe it. She put Molly in the car and headed to the store.
"I bought five pregnancy tests, went into a stall on Christmas Eve and peed on all five sticks and watched them all turn positive."
She called the doctor's office back: "I'm pregnant!" she told the nurse.
But in her 7th week of pregnancy, it all seemed to unravel.
"I was in the shower and it looked like 'Psycho,'" Ms. Nash said.
She was covered in blood.
"I started praying. I was losing both my children. Molly was going to die and we had no time, and everything Molly wanted in the world" - her own life, a little brother - was slipping away.
The infant's placenta had torn. Lisa spent the rest of the pregnancy in bed.
In March, 2000 a bone-marrow biopsy showed Molly's cells were pre-leukemic. At the end of June, another biopsy revealed worse results. If Lisa would agree to deliver early, she could save Molly now.
"I said, 'Absolutely not.'"
In late August, "Adam was born with a scream that cracked the walls. It was the most beautiful sound I ever heard."
Doctors examined the newborn, collected Adam's cord blood, and gave Molly her new stem cells a month later.
Today, Molly is 10 years old and in fourth grade.
"She's doing perfect," Lisa said. She still has Fanconi, she still requires tube feeding, "But her blood and bone marrow are healthier than mine are, and there's nothing she cannot do if she puts her mind to it."
Adam, the baby who saved her, is a happy 4-year-old. A third baby born of IVF, Delanie, is 18 months.
The Nashes were the first people in the world to use preimplantation genetic diagnosis to save another child. They make no apologies for their oft-criticized decision.
"Until they've been where I've been, and watched their child die slowly, day by day by day … until they've walked in my shoes, they'll never know what they would do. If you don't believe in it, don't do it. But don't judge me," Lisa said.
The process didn't hurt Adam at all.
"He was sort of like the pot of gold at the end of the rainbow," she said. "We had Adam so we could have Adam. The fact that he could help keep his sister here was sort of icing on the cake."
For Joe and Jennifer Makhlouf, using preimplantation genetic diagnosis was a simpler matter.
The couple tried for three years to have a child before turn
ing to fertility treatment. A year of fertility drugs didn't help.
"All of my friends were having their first babies. My sister had just gotten pregnant with twins. His brother's wife just got pregnant. Everybody was pregnant but us," Jennifer said. The couple was heartsick.
So they turned to in vitro fertilization. It wasn't a simple choice. They are Catholic. The church opposes assisted reproduction.
Not all Catholic couples take this prohibition as seriously as the Makhloufs. But they were torn between their ache for a baby and their strong loyalty to their church. They sought counsel from a priest.
Pray about it, the priest said. Look for God's guidance.
They decided to go forward.
"It's in God's hands," Joe said. "God is guiding the surgeon's hands." But they made one promise to themselves: no embryo would be destroyed in their effort to have children.
Their first in vitro attempt failed. A second attempt brought a pregnancy, but their elation died with a miscarriage.
To determine why this healthy young couple could not carry a pregnancy to term, Dr. F. Nicholas Shamma, with IVF Michigan, which includes Toledo Fertility Center in Sylvania, sent them for genetic testing.
The test revealed a problem in Jennifer's chromosomes. One had a tendency to invert. The flaw killed embryos.
That's when Dr. Shamma suggested preimplantation genetic diagnosis. The couple's embryos would be screened, and only the ones capable of surviving a pregnancy would be returned to Jennifer Makhlouf.
The Reproductive Genetics Institute was closed when the Jennifer and Joe finally arrived in Chicago. They rang a doorbell. A man in a white coat met them at the door, took the little incubator from their hands, and walked away. Now, the waiting began.
Without PGD, couples learn of fetal defects only after a pregnancy is established. At that point, they can decide to abort, or prepare themselves for the special needs of their new baby.
It appears a growing number of couples abort.
There is little data on the subject, but one study by the U.S. Centers for Disease Control and Prevention published in 1994 shows an unexplained decline in the number of children born with Down syndrome to mothers 35 years and older. This is the age group with the highest incidence of Down syndrome babies, and also the one most likely to be offered prenatal testing for the chromosomal abnormality.
In this CDC study of 17 states, the number of Down syndrome babies dropped 29 percent, from 36.6 per 10,000 births in 1983 to 25.9 per 10,000 in 1990.
Other couples who carry genetic diseases often decide to forgo pregnancy rather than risk cystic fibrosis or sickle-cell anemia. PGD would allow them to make sure an embryo is free of such diseases.
Use of the technique increases as researchers develop more probes for specific diseases.
But some have grave ethical concerns about the practice.
Wesley J. Smith calls PGD "really dangerous," because of the kinds of selection it could, some day, permit. Mr. Smith is a lawyer and senior fellow at the conservative Seattle think tank, the Discovery Institute.
"What if they found homosexuality was genetically based?" he asked. "How many of those embryos do you think would make it to being born?"
He notes one survey that found 11 percent of respondents would abort a child that carried a genetic propensity to obesity.
But such concerns are premature. Most human behavior is the result of complicated interactions among many genes and the environment. Science has not identified the genes that make us intelligent, or antisocial, or simply taller.
But there are screens for some adult diseases that could have serious consequences, he said.
"What might have happened in past, if we were able to really genetically judge our children?" he asked.
"Some of the most powerful contributors to human welfare were people who had to go through significant difficulties," Mr. Smith said.
Abraham Lincoln was prone to depression, Mr. Smith said. Other great leaders struggled with alcoholism. Physicist Stephen Hawking has amyotrophic lateral sclerosis, also known as Lou Gehrig's disease. And what about Lou Gehrig himself?
Would the "This Land Is Your Land," have ever been written had Woody Guthrie's parents known he would die of Huntington's disease at 55?
Selection of embryos to avoid adult diseases is not about the child being created, Mr. Smith said, "but about us. We don't want to deal with it." These are choices that may take "away the best of us."
One of the more controversial uses of PGD is for sex selection.
The American Society of Reproductive Medicine, which represents most U.S. fertility doctors, recommends PGD for sex selection only to prevent sex-linked diseases.
But ASRM's position hasn't stopped fertility specialists from a broader use of sex selection. A few clinics advertise the availability of sex selection, and IVF Michigan, which includes the Toledo Fertility Center in Sylvania, allows it if, for instance, a family has three sons and wants a daughter, a practice called family balancing.
But Yury Verlinsky, director of the Chicago reproductive laboratory to which the Makhloufs took their precious embryos, said that a couple doesn't have to tell him they're doing sex selection. The embryos' sex is part of the report. Parents simply can chose without getting anyone's permission.
A few clinics offer PGD routinely. Mr. Verlinsky's lab has performed PGD on about 5,000 embryos that led to the births of 600 babies, he said. He believes the procedure reduces miscarriage rates among IVF patients from 80 percent to 15 percent. Mr. Verlinsky says this data will be presented at a conference soon. It is not published in a scientific journal.
"We offer it for 100 percent of our patients. We suggest it for everyone who goes through IVF," he said.
His clinic is unusual in its total advocacy for PGD. Joseph Karnitis of the Toledo Hospital Fertility Clinic advocates PGD only for patients with a history of specific genetic conditions.
The Toledo Hospital does not do the work itself, but refers the patients to other fertility laboratories.
But Dr. J. Ricardo Loret de Mola of the MacDonald Fertility & IVF Program, part of University Hospitals Health System in Cleveland, says there's little clear evidence that preimplantation genetic diagnosis improves pregnancy rates.
"The data is actually controversial," he said, and he worries the technique could harm normal embryos.
"It's a procedure that's never been studied, really, in longitudinal data. You have to digest a hole on the embryo. You expose the embryo to chemicals. You can do it with laser, but you're exposing the embryo to heat, heat that normally wouldn't be there. You have to extract one or two cells out."
Further, the technique is not a perfect predictor, Dr. Loret de Mola said.
"We think of this technology as foolproof. It is not foolproof. We really do not understand how the embryo works," he said.
When Jennifer and Joe Makhlouf dropped off their two embryos at the Reproductive Genetics Institute in Chicago, they just wanted to know if they could have a baby.
They tried to relax, spending a Saturday in Chicago shopping and visiting friends. But those two tiny embryos never were far from their mind.
"To tell you the truth, that whole week was just excruciating," Joe said, "just to await the outcome of our two precious embryos."
The laboratory promised to call the couple at noon on Sunday. The Makhloufs paced their cramped hotel room, seldom glancing out the single window into the snowy streets. Around 1:30, the phone rang.
The embryos were both normal. And they were both boys.
The couple went straight to the lab to retrieve the small incubator. Another nerve-wracking drive, this time through heavy traffic, brought them back to Michigan IVF after dark. A doctor met them in the parking lot. He took the box, and the Makhloufs went home for a restless night's sleep.
The next morning, they were at the clinic before 9. In the two days since they left for Chicago, the embryos had grown to 100 cells. Doctors carefully returned them to their mother's womb. Everyone held their breath.
Today, their son, Anthony is nearly a year old. He sits on dad's lap, giving his guests intensely focused scrutiny before looking for something more interesting.
"We go to bed every night and our last words to each other before we go to sleep are about how cute Anthony is," Jennifer said.
"The day after I delivered him, I was going down the hall to get a drink. I heard all the other babies in the ward crying, and I came back and said, 'Joe, our baby cries the cutest.'"

No comments:
Post a Comment