
1st April 2008
I had a 'saviour sibling' to cure my desperately ill son - but now I've found out my newborn daughter can't save his life
By HELEN WEATHERS
Donna Zammit's first, tearful words to her husband Thomas after their baby daughter was born six weeks ago were: "I did this for Jamie."
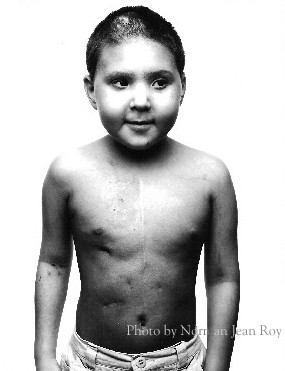
Strange words, but then baby Donatella was conceived with the primary intention of her becoming a "saviour sibling" to her nine-year-old brother Jamie, who suffers from the rare genetic blood disorder Fanconi anaemia.
Their unbridled optimism that Donatella might provide their son with a bone marrow transplant and in doing so save his life has been cruelly short-lived.
Two weeks ago the Zammits received the devastating phone call from Great Ormond Street hospital in London to say that tests on Donatella's umbilical cord blood had revealed she was not a perfect tissue match for her brother.
She will not save Jamie's life and although Donna and Thomas say they love Donatella just the same, inevitably her birth has been tinged with disappointment.
Mother-of-five Donna, 36, still hasn't broken the devastating news to Jamie, who is already struggling to cope with the physical and emotional effects of the disease, for fear it will emotionally crush him.
She doesn't regret having Donatella, but in her darker moments she questions the wisdom of raising her son's hopes by telling him, before she fell pregnant, she was going to try for a "saviour sibling".
"The time just never seems to be right to tell him," says Donna, a former advertising PA who lives with Thomas, 33, a shop manager in Bromley, Kent.
"The hospital keeps asking me: 'Have you told Jamie yet?' but I don't want to upset him.
"I felt such a failure when we found out that Donatella was not a perfect match, because we'd been so hopeful and quietly optimistic.
"When I first told Jamie I was going to try for a baby to help save his life, his reaction was: 'That's great, mum.'
"He was so sweet and caring when I was pregnant with Donatella and since her birth
"He loves holding his little sister in his arms, stroking her head and kissing her little fingers, and I keep thinking: 'Will he feel the same way about her when he knows she can't help him?'"

And it is this pertinent question which goes to the heart of the controversial ethical debate about "saviour siblings" or, more brutally, "spare part" babies.
To what extent are Jamie's feelings towards his sister coloured by the knowledge she was conceived in the hope of saving his life? Will he end up resenting her for not being able to do so?
And how will Donatella feel, growing up knowing she might not have existed had her brother not needed a bone marrow transplant?
Will she feel as much a failure as her mother, for failing in this one vital respect, and believe herself to have let down both her parents and her brother?
Children diagnosed with Fanconi anaemia, or FA, are generally not expected to survive beyond their teens or early 20s, and if no bone marrow donor is found, will Donatella feel the burden of guilt fall on her small shoulders?
These are tough questions that Donna and Thomas admit have exercised their thoughts daily.
The truth is, they don't know if what they tried to do was right or wrong, they are simply desperate to save Jamie's life.
"I love Donatella as much as my other children. I love her for herself and not for what she might have been able to do for her brother, so while there is a disappointment, I am not disappointed with her," says Donna.
"I don't know if what I tried to do was right or wrong, but until people have stepped into my shoes and lived with the reality of having a very sick child, they have no right to judge.
"As a mother I feel I have a duty to try to do everything I can to try to save my son's life and I believe any mother in the same situation would feel the same way."
Britain's first saviour sibling was born in June 2003 to a couple who were desperate to cure their young son of a rare form of anaemia.
Jamie Whitaker was genetically matched as an IVF embryo to his brother Charlie, who was four years old at the time.
His parents Jayson, 37, and Michelle, 35, from Derbyshire, travelled to Chicago for the specialised treatment - which was a success - after being refused permission to select a tissue-matched embryo by Britain's Human Fertilisation And Embryology Authority.
In July 2004 the HFEA became the first in the world to officially sanction the practice, saying such treatment could benefit the whole family, and in April 2005 the House of Lords ruled that the creation of designer babies to treat brothers and sisters with life-threatening disorders was lawful.

This followed their upholding of a 2003 High Court judgment which granted a couple from Leeds, Raj and Shahana Hashmi, the right to use controversial fertility treatment to select an embryo which could help save the life of their son Zain, then aged six, born with a fatal genetic blood disorder.
Mrs Hashmi, now 43, had a series of unsuccessful attempts at IVF, failing either through miscarriage or because an embryo with the right tissue group was not produced.
In January the House of Lords further approved proposals in the Human Fertilisation and Embryology Bill - which recently sparked a furious row between politicians and the Catholic Church - allowing parents to use saviour siblings to treat serious and potentially life-threatening ailments.
These could include conditions such as sickle cell anaemia, renal failure, kidney disease and spinal diseases.
Needless to say, Donna supports the bill wholeheartedly despite the uncomfortable issues it has thrown up in her family.
She does not intend to use IVF in a further attempt to save her son's life, by conceiving a designer baby as opposed to relying on nature.
"I have five children, one with Fanconi anaemia, and I think to have another would put too much strain on my health - I want to be around to help Jamie," she says. "Our only hope is a bone marrow transplant from a donor."
Donna says she would have loved the opportunity to have IVF - virtually guaranteeing a perfect match for her son - but received negative replies from almost every clinic she approached before she fell pregnant with Donatella, on ethical grounds.
With, campaigners and Catholic Church leaders argue, good reason.
Is it ethical to deny a child the choice over how its body is used? Could that child then be called upon to provide further "spare parts" against its will?
Church leaders are demanding the Government allow MPs a free vote on the bill, based on conscience, and have decried the creation of designer babies, and the destruction of embryos rejected purely because they do not match the tissue of an existing ill sibling.
Surely this must trouble Donna's conscience?
"It took me a year-and-a-half to decide to have a fifth baby," says Donna, whose other sons Tommy, 11, Roberto, five, and Lorenzo, four, are perfectly healthy.
"Great Ormond Street hospital made some approaches to fertility clinics but everything was moving so slowly I decided to have a baby naturally.
"It was absolutely nerve-racking and there were times when I felt like we were playing God. We knew there was a one-in-four chance this baby might also be born with FA and that was a huge risk to take," says Donna, who along with Thomas is a carrier of the disease.
"I didn't know that I would be able to cope with another ill child, and the first 12 weeks of the pregnancy, until tests showed that she didn't have it, were the worst of my life. I felt sick with worry.
"Had Donatella inherited FA I think I would probably have had a termination.
"I love children and I don't believe it's right to end a life, but knowing how Jamie has suffered I also believe it's not right to put a child through that either.
"If we'd been able to have IVF, we would have been able to select an embryo which would have given us some certainty.
"We would have been able to tell Jamie he could have a bone marrow transplant instead of just hoping for it."
Jamie was six years old when Donna and Thomas first started to worry about his health. Always small for his age, he grew increasingly pale, lethargic and breathless after starting school.
Then living in Malta, where Thomas was born, Donna took Jamie to the hospital where tests revealed he had a red cell count of just 3.8, compared with a normal reading of 15 or 16.
Doctors suspected leukaemia, and because they did not have the facilities to investigate further, he was referred to Great Ormond Street hospital.
He went through a battery of tests and was diagnosed with FA in April 2005.
"When they told us Jamie had Fanconi anaemia I didn't know what they were talking about because I'd never even heard of it," says Donna.
"But I knew it was serious when they said his only hope was a bone marrow transplant. We were stunned, and my immediate fear was that our other sons had it too.
"They were all tested and the two weeks we had to wait for the results were the worst of my life.
"I kept looking at them, thinking: 'Have you got it, too?' I kept looking for signs I'd read on the internet and had started to convince myself they had them.
"When Great Ormond Street phoned up and said: 'Good news, Donna, your other sons don't have it,' I collapsed with relief.
"But poor Jamie would say: 'Why me and not my brothers?' He couldn't understand why he was the only one to have this disease.
"I explained to him that we, as parents, had no idea that we carried this disease until he was born and that there was nothing we could have done to prevent it.
"I told him that there are some things in life that we have no control over, but he was only six and to him it just seemed unfair.
"But I'm the kind of person who tries to face things head on and stay positive, so I thought: 'Right, we are going to find a donor and everything is going to be all right.' I was determined to do everything to help our son."
When Donna and Thomas started to research the disease, however, their spirits sank. FA is so rare that it is believed to affect only one in six-and-a-half million people. The number of carriers is between one per 100 and one per 300 of the population.
There are ten families in Britain with children who have the inherited disease, which affects the production of red blood cells, leading to aplastic anaemia.
This is accompanied by a whole host of other medical issues including skeletal problems, small head circumference, short stature, growth and development problems and misshapen or missing thumbs.
People with FA are also more susceptible to developing cancers, such as leukaemia, and organ tumours, and have compromised immunity to common ailments such as colds and infections.
Without a bone marrow transplant, the only treatment for Jamie is monthly blood transfusions or the steroid treatment oxymetholone, which raises the red blood count but has the side effect of bringing on early puberty.
"Jamie was diagnosed in April 2005 and we felt really confident that a bone marrow donor would be found," says Donna.
"Our other sons were tested, in the hope that one of them was a perfect match, but none of them were.
"That Christmas we were elated when Great Ormond Street hospital told us they'd found a female donor who was a nine out of ten tissue match.
"But our world caved in when they explained they would only use this donor as a last resort, if Jamie's condition really deteriorated, because he's in such a fragile state he needs a ten out of ten match for the operation to have a real chance of success.
"Even with a ten out of ten match the survival rate is 80 per cent, because before a transplant operation you have to undergo chemotherapy to dampen down the immune system, and for FA patients chemotherapy is especially toxic.
"So we've been searching for another donor but because Jamie has such a rare tissue type, it's been really hard.
When the staff at Great Ormond Street first mentioned that having another baby might provide a perfect match, my first reaction was to say: 'No way.'
"I felt I had enough to cope with, with four young boys and one who was very ill. It was just too much for me to take in.
"I talked it over with Thomas and he was keen for us to try, but it was me who was going to have to carry the baby and live with the fear that the new baby might also have FA."
What changed Donna's mind was the profound psychological effect FA was having on Jamie, who - as he grew older and understood more about the condition - became prone to depression.
"The drug therapy has also hastened the wild mood swings associated with puberty.
"Although Jamie goes to a mainstream primary school, he can't do all the things the other boys do, so he feels very isolated," says Donna.
"He bruises like a peach and even the slightest graze could lead to a serious infection.
"The steroid treatment has brought on early puberty and all his friends at school keep asking: 'Why has Jamie got such big muscles?' and 'Why is he growing a moustache?' He doesn't like being different from everyone else.
"He has become very easily upset and confrontational at home. Recently he ran upstairs saying: 'I wish I was dead, I wish I had never been born,' and I didn't know how to comfort him.
"All we can do is try to stay positive, make sure he feels loved and distract him with fun activities.
"He won't even talk about his condition now and whenever the hospital or haematologist phones up with the latest blood test results he'll say: 'I don't want to know,' before running off to his room.
"I love all my children equally and treat them all the same, but what mother wouldn't want to do anything in their power to stop their child's suffering?
"That was why I decided to have another child. I'm one of seven children and I always wanted a big family, so I reasoned that maybe I was simply bringing forward the child I was always going to have.
"After my youngest son Lorenzo was born, I certainly never said: 'That's it, no more.'
"I was always open to the idea of more, but Jamie's situation made me think a bit harder. For me, it was a risk worth taking.
"When I became pregnant with Donatella, all the staff at the hospital were so excited for us.
"They care so much for Jamie and I think everyone really thought that this baby would be a perfect match.
"There was a one in four chance of that happening and having had three sons who weren't a match, I thought: 'Surely this one must be?'
"Every time I went to the hospital the nurses would ask: 'When's the baby due?' which made it even worse when I had to tell them that Donatella was not a match and that we were still looking for a bone marrow donor."
A much loved and wanted sibling Donatella may be, but she is not the saviour they all hoped for. How this will affect the dynamic of the family, only time will tell.

No comments:
Post a Comment